The passage of a kidney stone is often described as one of the most painful experiences one can endure; possibly even more so than childbirth. In addition, stones that do not pass can lead to blockage of the kidney, risking loss of organ function if left untreated. Most seriously, a urine infection in this setting can be life-threatening and constitutes a medical emergency.
In addition, patients lose a tremendous amount of time away from their jobs, significantly impacting their earning potential.
Luckily, with appropriate, modern treatment, the success rate of timely intervention is quite high, approaching 95 to 100 per cent.
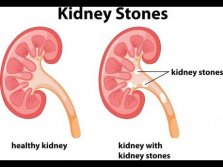
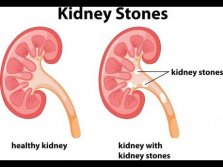
SYMPTOMS OF URINARY STONES Many stones may remain silent until they grow to block the urinary system. The patient may complain of severe back or groin pain; they may have burning on urination or see blood in the urine. Nausea and vomiting are common, and fever and chills with pain are signs to take seriously, as they most commonly indicate an infection. A medical evaluation is essential if any of these are experienced. An X-ray, ultrasound or CT scan may be ordered by the physician to confirm the diagnosis and plan intervention.
MANAGEMENT OPTIONS The modern approach to urinary stone disease is centred around non- and minimallyinvasive procedures; that is, surgery without a large, painful incision (or ‘cut’ to the body). To this end, the use of scopes and camera systems that offer an internal view into the organs of the patient is incorporated. Then, utilising energy sources such as lasers, ultrasound and shock waves, the stones are broken up and can then be removed or passed painlessly. These approaches can be applied to stones of all sizes and complexities, resulting in faster recovery times (most times patients are back to work the next day), with almost no pain experienced after surgery, and far higher successful stone-removal rates compared to open surgery. In addition, the complication rates are far lower with these techniques.
IS SURGERY ALWAYS NECESSARY? The probability of a stone passing without any intervention is highly dependent on its size and location.
Small stones less than one cm may remain silent and cause no trouble. However, the probability that these stones progress to cause pain or obstruction is around 75 per cent. Larger stones are highly likely to produce complications, and should be actively treated rather than observed.
There are specific situations in which surgery is absolutely mandatory, in which it would be a great hazard to health and life should surgical intervention not be executed. In particular, a urinary tract infection (associated with burning with urinating, feeling generally unwell or weak, or a fever), impairment of kidney function, or a high level of obstruction seen on imaging, demand emergency intervention.
DIETARY AND LIFESTYLE CHANGES Once someone has had a urinary tract stone, they will always be at risk of forming a stone again. The lifetime risk of stone recurrence is approximately 50 per cent. However, there are dietary and lifestyle alterations that decrease one’s chances of having stones again in the future. Obesity is a significant risk factor, and losing weight is associated with decreased chances of stone formation.
A minimum daily intake of water of two litres is recommended. In addition, salt intake should be reduced, especially by decreasing preserved food products which are high in sodium. Citrate has a protective effect on stone formation; it is recommended that stone formers squeeze fresh lemon juice, which is high in this chemical, into their water on a daily basis.
More specific dietary advice comes from analysis of the stone fragments obtained during surgery.
AN EXCITING TIME IN STONE SURGERY Never before has it been easier, safer and more convenient to have urinary stones treated. With the wide array of surgeries available, specifically tailored to each individual stone and patient, the heavy impact of stone disease can been softened.